What Is Medical Misconduct?
Medical misconduct refers to unethical, negligent, or abusive actions by healthcare providers that violate professional standards and harm patients. It goes beyond traditional medical malpractice and includes ethical, sexual, and professional violations by doctors, nurses, therapists, and other licensed professionals.
Misconduct occurs when a provider acts, or fails to act, in ways that breach medical ethics, legal duties, or patient trust.
This guide explains the major types of medical misconduct, relevant laws and reporting rules, hospital and institutional liability, and the legal options available to victims seeking accountability and compensation.
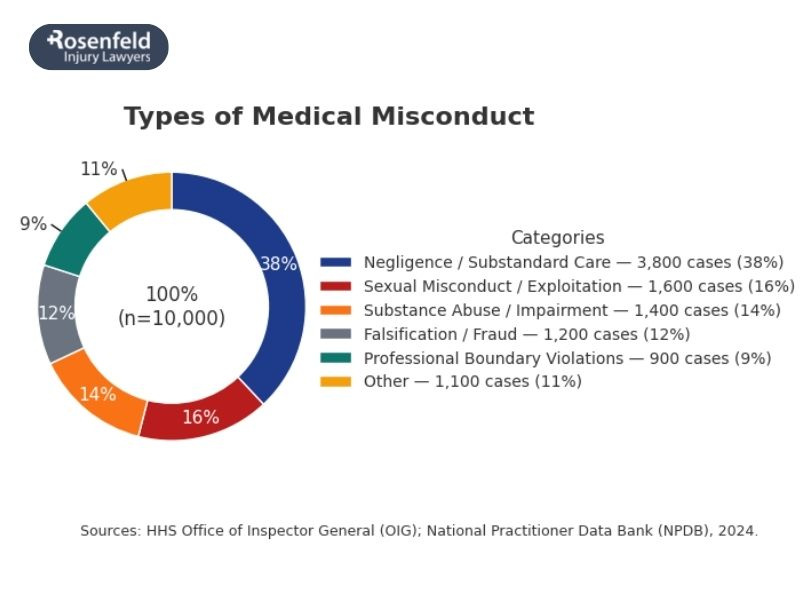
What Are the Types of Medical Misconduct?
Patients place immense trust in their doctors, nurses, and therapists, trusting them with their bodies, health, and often their lives. Medical misconduct represents a profound betrayal that can cause lasting emotional and psychological trauma as well as serious consequences.
Sexual Misconduct
Sexual misconduct is among the most devastating forms of medical misconduct. It includes:
- Sexual assault, coercion, or exploitation during treatment or examinations.
- Inappropriate touching, sexual comments, or exams without informed consent.
- Boundary violations disguised as legitimate medical care, such as unnecessary exposure or invasive procedures.
Medical Negligence or Fraud
Some healthcare providers engage in misconduct for financial gain or due to reckless disregard for patient safety. Examples include:
- Performing medical procedures without consent or outside one’s area of competence.
- Falsifying medical documents or billing for unnecessary tests, surgeries, or treatments.
- Improperly prescribing controlled substances or participating in kickback schemes.
Substance Abuse or Impairment
Medical professionals have a duty to provide safe, competent care. That obligation is violated when they:
- Practice medicine while impaired by alcohol, illegal drugs, or prescription misuse.
- Fail to disclose or seek help for a substance dependency that puts patients at risk.
Abuse or Exploitation of Vulnerable Patients
Some forms of misconduct target those least able to defend themselves, including the elderly, disabled, or institutionalized. This includes:
- Verbal, emotional, or physical abuse of patients under medical care.
- Neglect or willful mistreatment in hospitals, nursing homes, or residential treatment facilities.
Boundary Violations
Professional boundaries are essential to patient trust. Misconduct occurs when doctors and surgeons:
- Form personal, romantic, or sexual relationships with current patients.
- Exploit confidential medical information for personal gain or manipulation.
Each of these forms of misconduct violates the ethical core of medicine, to do no harm, and may give rise to civil, criminal, or administrative consequences for the provider involved.
What Are the Key Differences Between Medical Malpractice and Negligence?
While often used interchangeably, medical malpractice and medical negligence differ in intent and severity.
Medical negligence happens when a healthcare provider fails to use reasonable care, causing harm through error or omission. It usually involves mistakes such as:
- Misdiagnosis or delayed diagnosis
- Wrong medication or dosage
- Surgical or monitoring errors
- Lack of informed consent
Negligence is typically unintentional, but still a serious breach of professional responsibility.
Medical malpractice is a legal claim that arises when a provider’s actions fall below the accepted standard of care and directly cause harm or death. It can include:
- Ignoring test results or symptoms
- Performing procedures beyond one’s competence
- Reckless or unethical treatment decisions
In short, all malpractice involves negligence, but not every negligent act qualifies as malpractice. Both can lead to devastating consequences and may entitle victims to pursue a lawsuit to seek damages.
How Common Is Medical Misconduct?
According to a study published in BMJ, medical errors are estimated to cause more than 250,000 deaths each year, making them the third leading cause of death in the U.S., after heart disease and cancer. Even though medical misconduct is widespread, it is often hidden due to underreporting, confidentiality laws, and limited oversight.
According to the NCBI, about 1 in 3 clinicians will face a medical malpractice lawsuit during their career, showing how often patients allege serious harm or unethical care.
RAINN estimates that only 5–10% of victims of sexual abuse by healthcare professionals ever report it. Between 2003 and 2013, the National Practitioner Data Bank logged 1,039 reports of physicians accused of sexual misconduct, and from 1999 to 2015, over 3,100 doctors were publicly disciplined. In a review of 101 abuse cases, 89% of victims were women.
Among medical students, 12.2% reported nonconsensual sexual contact during training in a 2023 study.
Experts agree these numbers represent only a fraction of real cases. Many hospitals handle complaints internally, allowing repeat offenders to continue practicing and leaving victims without justice.
What Laws Govern Medical Misconduct?
Medical misconduct can violate civil, criminal, and administrative laws at both the federal and state levels. These laws exist to protect patients’ rights, ensure accountability, and uphold professional and ethical standards within the medical field.
Health Insurance Portability and Accountability Act (HIPAA) — 42 U.S.C. § 1320d
HIPAA protects patient privacy and governs how healthcare providers use and share medical documents and personal health information. Violations, such as disclosing private details or misusing data, can result in civil penalties, fines, and even criminal prosecution.
Civil Rights Act – Section 1983 — 42 U.S.C. § 1983
This statute allows patients in public hospitals, prisons, and state-run facilities to sue state-employed providers for constitutional violations, including deliberate indifference, abuse, or denial of medical care.
False Claims Act — 31 U.S.C. §§ 3729–3733
The False Claims Act prohibits billing fraud, false documentation, and kickback schemes involving federal programs like Medicare and Medicaid. Healthcare providers who submit fraudulent claims can face steep fines and treble damages.
Prison Rape Elimination Act (PREA) — 31 U.S.C. §§ 3729–3733
PREA establishes national standards to prevent and address sexual abuse of patients in correctional, detention, or state-operated medical settings. It applies to both medical and custodial staff working with vulnerable populations.
State Medical Practice Acts and Licensing Boards
Each state has its own Medical Practice Act, which defines unprofessional conduct and empowers state medical boards to investigate, discipline, or revoke licenses for misconduct. These acts typically cover issues like negligence, sexual abuse, substance impairment, falsifying records, and boundary violations.
What Consequences Do Medical Professionals Face for Misconduct?
The consequences of medical misconduct vary depending on the nature of the violation, the harm caused to the patient, and whether the act breached criminal law, ethical codes, or medical board standards.
Disciplinary Action by Medical Boards
Most cases of misconduct begin with an investigation by a state medical board or licensing authority. “Disciplinary action” refers to administrative penalties meant to protect the public from unsafe practitioners. Common sanctions include:
- Written reprimands or letters of concern
- Probation or mandatory supervision
- Required retraining or ethics courses
- Monetary fines or temporary suspension
Even if no criminal charges are filed, disciplinary measures help ensure that providers who violate professional standards face accountability and oversight.
Revocation or Suspension of a Medical License
In more serious cases, such as sexual abuse, patient injury, or drug diversion, the medical board may suspend or permanently revoke a provider’s license.
The process typically follows a set path:
Complaint → Investigation → Administrative Hearing → Sanctions (revocation, suspension, or voluntary surrender).
Losing a medical license can effectively end a provider’s career and prevent them from practicing in other states through data-sharing systems like the National Practitioner Data Bank.
Criminal Charges
When misconduct rises to the level of a crime, healthcare professionals may face felony prosecution. Examples include:
- Sexual battery or assault by a healthcare provider (state-specific statutes)
- Prescription drug diversion under 21 U.S.C. § 841
- Medicare or Medicaid billing fraud under the False Claims Act
Criminal convictions can result in imprisonment, fines, restitution, and mandatory reporting to federal and state authorities.
Civil Liability
Victims of medical misconduct also have the right to file civil lawsuits seeking compensation for injuries, trauma, or exploitation. Claims may include:
- Medical negligence or malpractice, including medical errors, surgical errors, medication errors, and other forms of incompetence
- Battery or intentional infliction of emotional distress
- Institutional liability against hospitals or clinics for negligent hiring, supervision, or failure to report known misconduct
These civil actions help survivors recover financial relief and serve as a vital tool for enforcing accountability across the medical profession.
Who Can Be Held Liable for Medical Misconduct?
Liability for medical misconduct can extend beyond the individual provider to include the institutions and organizations that allowed the misconduct to occur or failed to prevent it.
- Hospitals and clinics can be held liable for negligent hiring, retention, or supervision, and may face vicarious liability for employee misconduct during the course of employment.
- Medical corporations or group practices may be sued for failing to establish safeguards, ignoring complaints, or prioritizing profit over safety.
- State licensing boards can, in rare cases, face claims for failing to discipline known offenders when public safety was compromised.
- Third-party contractors such as staffing agencies, traveling nurses, or telehealth providers may share liability for negligent credentialing or supervision.
- Religious or institutional facilities, including faith-based hospitals and rehabilitation centers, can be held responsible for institutional negligence or vicarious liability, similar to clergy abuse cases.
What Legal Options Do Victims of Medical Misconduct Have?
Victims of medical misconduct have several legal paths available, depending on the type and severity of the wrongdoing. Each serves a different purpose, from punishing offenders to compensating victims and preventing future harm.
- Criminal proceedings: Patients can report sexual abuse, assault, or healthcare fraud to law enforcement or the state Attorney General’s office. These cases may lead to criminal charges, imprisonment, fines, or loss of medical licenses.
- Civil lawsuits: Patients may file a medical malpractice lawsuit or other civil claim against the provider, hospital, or institution to demand financial recovery for physical and emotional trauma, financial losses, and other damages. Civil actions often deliver a sense of accountability and justice that criminal or administrative processes alone cannot provide.
- Administrative complaints: Patients can report misconduct to their state medical board, which can investigate and impose disciplinary actions such as suspension, probation, or license revocation.
What Damages Can Victims Recover in Medical Misconduct Lawsuits?
Victims of medical misconduct can pursue damages to restore what was lost and recognize the profound physical, emotional, and financial toll of a provider’s misconduct.
Common recoverable damages include:
- Medical expenses: Costs of corrective medical treatment, hospitalization, therapy, or long-term care.
- Lost income and future earnings: Reimbursement for time away from work or permanent disability.
- Pain and suffering: Recognition of physical pain, emotional trauma, and diminished quality of life.
- Emotional distress and psychological harm: Especially significant in cases involving sexual abuse, exploitation, or betrayal of trust.
- Punitive damages: In extreme cases, additional sums may be awarded to punish willful, reckless, or malicious conduct and deter similar acts.
Statutes of Limitations
Each state sets a statute of limitations, a time limit for filing medical misconduct lawsuits, usually one to three years from the incident or its discovery. Some states extend this for cases involving fraud or concealment.
For sexual abuse or assault, many states now have delayed discovery rules or lookback windows allowing survivors to sue years or decades later. In some states, child sexual abuse claims have no time limit at all.
Because these laws vary, victims should consult an attorney promptly to understand the deadlines that apply to their case.
How to Report Medical Misconduct
Victims of medical misconduct should act quickly to protect their rights and help restore their well-being, as well as prevent further harm. Here’s a clear step-by-step guide:
- Report to the hospital or clinic. Contact the patient safety officer or hospital administration to file a written complaint and request a copy for your records.
- File a complaint with your state medical board. Each state board investigates reports of misconduct and can discipline or revoke a provider’s license.
- Report sexual abuse to law enforcement or HHS. In cases of assault or exploitation, contact local police or the Department of Health and Human Services for further investigation.
- Preserve evidence. Keep medical records, billing statements, emails, and witness information. Document dates and details while events are fresh.
- Seek trauma-informed support. Reach out to medical and legal professionals experienced in misconduct and negligence cases for guidance and protection of your rights.
How Injury Lawyer Team Can Help
At Injury Lawyer Team, we understand how devastating it is to experience medical misconduct, especially when it comes from someone you trusted with your health and well-being. You’re not alone, and you don’t have to face powerful hospitals or insurance companies on your own. We stand with victims who have been harmed, ignored, or betrayed by the medical profession.
Our sexual abuse and assault law firm helps clients by:
- Investigating hospitals, clinics, and medical boards to uncover what went wrong and who allowed it to happen.
- Working with trusted medical experts to identify negligence, unethical behavior, or abuse that caused harm or trauma.
- Pursuing claims against institutional defendants, including hospitals and corporations, even when immunity laws or complex procedures make the process difficult.
- Protecting clients’ privacy through compassionate, confidential representation focused on healing and accountability.
We operate on a contingency-fee basis, which means you pay nothing unless we win your case. Our consultations are always free and completely confidential.
If you or someone you love has suffered from medical misconduct, we’re here to listen, guide you through your options, and fight for the justice you deserve, with care, dignity, and compassion.
All content undergoes thorough legal review by experienced attorneys, including Jonathan Rosenfeld. With 25 years of experience in personal injury law and over 100 years of combined legal expertise within our team, we ensure that every article is legally accurate, compliant, and reflects current legal standards.








